Plantar fasciitis is one of the most common causes of heel pain, affecting millions of individuals every year. This condition can be debilitating for those who love to stay active and can make even the simplest of tasks, like walking, a daunting challenge. In this blog post, we will delve into what it is, the anatomy involved, how plantar fasciitis forms, diagnostic methods, treatment options, how to desensitize it, and techniques/exercises along with preventive measures to help one manage the condition effectively.
What Is Plantar Fasciitis?
The diagnosis “plantar fasciitis” encompasses disorders ranging from acute inflammation to chronic fibrotic degeneration, usually involving the heel attachment region. The primary function of the plantar fascia is to provide support to the arch of the foot, acting as a shock absorber but also providing support during activities like walking and running. When this fascia becomes overloaded or strained, it can develop small tears, leading to pain and discomfort, typically on the underside of the heel.
Anatomy Affected by Plantar Fasciitis
To fully understand plantar fasciitis, it’s important to recognize the key anatomical components involved:
- Plantar Fascia: This fibrous band of connective tissue supports the arch of your foot. Its role is crucial during walking, running, and jumping.
- Heel Bone (Calcaneus): The plantar fascia originates at the heel bone and runs along the bottom of the foot. Inflammation here is often where the pain is most palpable.
- Arch of the Foot: The plantar fascia provides structural support to the arch. Flat feet or high arches can predispose individuals to plantar fasciitis.
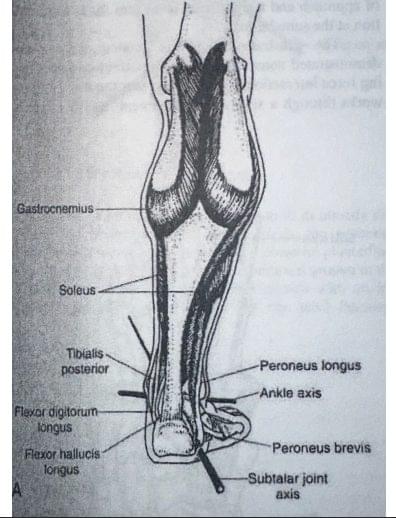
- Surrounding Muscles and Tendons: Other structures, including the Achilles tendon at the back of the ankle and various foot muscles, play a role in foot mechanics and can be affected if plantar fasciitis is left untreated.
How Does Plantar Fasciitis Form?
Plantar fasciitis typically occurs due to decreased ankle dorsiflexion and gastrocnemius tightness causing the heel to leave the ground prematurely during the gait cycle. This repetitive motion creates hypersensitivity on the foot arch which usually is most present in the morning when one is taking their first steps of the day, but also when they have been seated for a prolonged time frame and begin load-bearing through the walking phase. Several factors have been known to contribute to the condition, including foot structure: Flat feet, high arches, or an abnormal walking pattern placing excessive stress on the plantar fascia. This is not always true as systematic reviews have proclaimed. High-impact activities such as running, especially on hard surfaces, and other high-impact sports can place strain on the foot which exacerbates gastrocnemius tightness and ankle movement limitation. The common age range for plantar fasciitis is between 40-65 years although young athletes and runners have been less commonly known for developing PF. Excess weight also can add strain to the plantar fascia, increasing the risk of injury prevalence. Occupational risk can be considered if current anatomical and biomechanical complications occur in those with jobs that require standing for long periods.
Diagnosing Plantar Fasciitis
Diagnosing plantar fasciitis generally involves several steps:
- Medical History: A comprehensive assessment that considers your symptoms, any previous foot injuries, and lifestyle habits will be conducted.
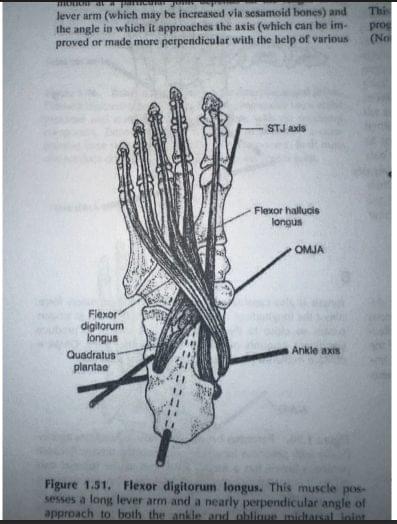
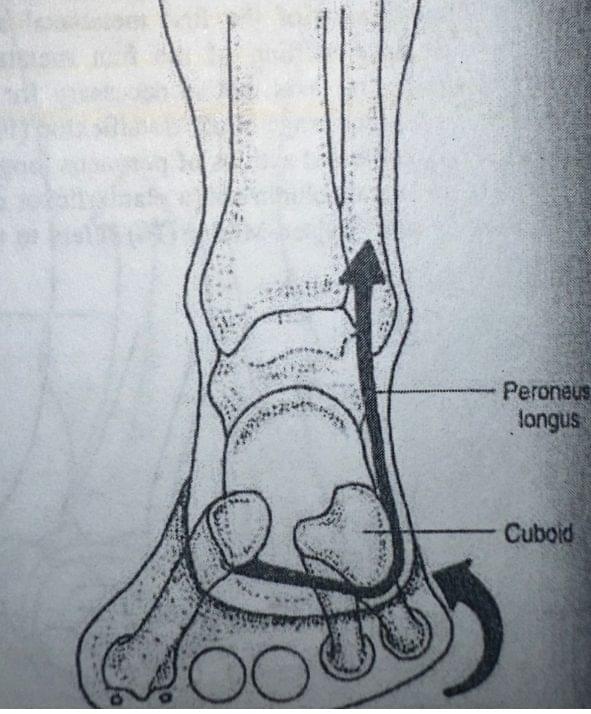
- Physical Examination: A healthcare provider will examine your feet and assess your walking pattern. They may seek specific areas of tenderness, especially around the heel. One of the most common factors to consider with the risk and diagnosis of plantar fasciitis is weakness of the peroneal and flexor digitorum longus/brevis tissue
- Orthopedic Tests: Windlass testing- The big toe is passively bent backward (dorsiflexed) while the heel bears weight; pain at the heel’s bottom signifies a positive test.

Treatment: Desensitization Techniques
Desensitization of plantar fasciitis is vital for recovery and often involves a combination of the night splint used throughout sleep for gastrocnemius stretch and tissue slack, along with the use of a racket/lacrosse ball for arch compression (rolling) while seated. The stated splint device helps to keep your foot in a dorsiflexed position, reducing morning pain and stiffness of the arch.
Passive and Active Exercises for Plantar Fasciitis Incorporating both passive and active exercises into your rehabilitation routine is essential.
Passive Exercises:
- Calf Stretches: Lean against a wall, placing one foot behind you with the heel firmly on the ground. Lean forward with both knees bent at 10-20 degrees holding for 45-60 seconds 4-5 sets. Repeat several times for each leg.
- Plantar Fascia Stretch: While seated, cross one leg over the other and pull the toes towards your shin with one hand and hold the base of the heel with the other hand to stretch the plantar fascia. Hold for 45 seconds and perform 3-4 sets.
- Stair foot stretch: Hang heels of edge of stair and drop heel below stair level and hold for same time and sets as #1. We understand that his is a decent investment of time but thousands of studies dating back to the 1990’s reflects considerable proof that static stretching such as the stated ones above are some of the best for building tendon resiliency and stifling sensitivity. DO NOT PERFORM THSE DAILY. Every 2-3 days is the recommended frequency for these stretches.
Active Exercises:
- Big Toe Lifts: While seated, lift your big toes while keeping the other 4 on the ground before dropping the big toe and lifting the 4 repeatedly. This helps strengthen the small muscles in your feet generally found to be weak and hard to engage.
- Heel Raises: Stand on the edge of a step with your heels hanging off. Raise your heels by pushing through the balls of your feet and pressing the toes down before lowering the heels back down. Repeat several times.
- Arch Lifts: While standing, try to lift your arch while keeping your toes and heel on the ground. This promotes strength without excessive strain.
- Peroneal Strengthening: Place a band around both feet while seated and bring the feet apart for band tension. With straight legs, lift the outside of the feet up and down in repetition so the peroneal muscles close to the outer calf get engaged.
Footwear Considerations for Plantar Fasciitis
Your choice of footwear can significantly affect your symptoms. Here are some guidelines:
- Arch Support: Choose shoes that provide excellent arch support to help reduce the strain on the bottom of the feet.
- Cushioning: Look for inserts with adequate cushioning to absorb shock during walking and running.
- Stability: Shoes that offer good stability can help maintain proper alignment and reduce stress on the foot.
- Avoid Flat Shoes: Flip-flops and flat sandals offer little to no support and should generally be avoided if you’re dealing with plantar fasciitis. Flat footwear will continue to aggravate symptoms during your treatment process, prolonging the desensitizing process.
Preventing Plantar Fasciitis in the Future
While some factors contributing to plantar fasciitis are unavoidable, several proactive measures can help mitigate the risk:
- Maintain a Healthy Weight: Keeping your weight in check can reduce stress on the feet.
- Choose Supportive Footwear: Invest in quality shoes, especially if your job or lifestyle requires prolonged standing or walking.
- Stretch the feet, legs and hips regularly: Incorporate foot, calf, hamstring and hip stretches into your daily routine, especially before and after physical activities.
- Gradual Increase in Activity: When starting a new exercise or sport, gradually increase the intensity and duration to allow your body to adapt.
- Cross-Train: Engage in low-impact exercises such as swimming or cycling to maintain fitness while temporarily reducing pressure on your feet.
- Listen to Your Body: If you begin to feel discomfort, don’t push through the pain. Take breaks, perform the previously stated protocol and seek treatment as necessary.
Final Thoughts
Plantar fasciitis may be a common ailment, but that doesn’t mean you have to suffer through the pain and limitations it can impose. With the right knowledge and strategies for diagnosis, treatment, and prevention, you can effectively manage this condition. By understanding the anatomy involved, being proactive with exercises and footwear, and utilizing desensitization methods, you can achieve a pain-free experience in the future. If you are noting symptoms of plantar fasciitis, consult HIS professionals who can provide you tailored advice and guidance. Your feet carry you through life, so treat them right! For any additional queries or personalized assistance, please reach out to us at Integrated Health Solutions. We’re here to help you get back on your feet!
Content Provided By Dr. Parker Grundman













